This article was originally published in the 2019 Spring Issue, and can be read here.
Authors: Wylie Barker, Nardin Farag, Yae Eun Lee, Haroon Munir, Chloé Pierret, Yiqing Xia, Candace Yang
Universal health care is often seen as a distant dream for many low- and middle-income countries, but for Thailand, it was achieved through the implementation of its Universal Coverage Scheme (UCS). By 2001, nearly 18 million people were falling through the cracks of Thailand’s healthcare system, serving as the main driving force behind the establishment of the UCS. After implementation of this scheme in 2002, 47 million people received coverage, equating to approximately 75% of the country’s population. The goal of the UCS was to entitle all citizens to quality health care regardless of socioeconomic status, and the scheme provided beneficiaries with a comprehensive benefits package focused on primary health care. Although the impact of the UCS was significant, disparities between rural and urban areas prevail. This case study assesses the impact that implementation of UCS had on the utilization of healthcare in rural areas compared to urban ones by examining health service utilization, rate of catastrophic health expenditure, health indicators, and quality of care. The UCS ultimately increased healthcare coverage for all Thais, but the perpetuated inequity between rural and urban areas remains a persistent issue, demanding the prioritization of equal distribution of resources.
Background and Motivation
Prior to the introduction of the Universal Coverage Scheme (UCS), Thailand had four public health insurance programs that covered the entire population: The Civil Servant Medical Benefit Scheme (CSMBS), the Social Security Scheme (SSS), the Medical Welfare Scheme (MWS), and the Voluntary Health Card Scheme (VHCS) (1). The CSMBS covered people in the government employment sector, including their dependents and retirees, while the SSS covered private sector employees (1). The MWS was a free health insurance program for socially vulnerable people and covered the poor, the elderly, the disabled, and children under 12 years of age (1). Finally, the VHCS was a voluntary program for those ineligible for the other three programs; it allowed each household to purchase one year of coverage for 500 Baht (approximately $15 USD) (1).
The MWS and VHCS faced administrative issues that left approximately 18 million people (nearly 30% of the population) uninsured, and these were mostly informal sector workers from lower socioeconomic groups (1). The MWS encountered mistarget difficulties in assessing the incomes of people in the informal employment sector. This resulted in MWS cards tending to be distributed to the non-poor rather than the poor (1). In addition, the VHCS faced an adverse selection issue, where illness was positively correlated with purchase and utilization of the VHCS insurance card (1).
Hence, the driving force behind the decision of the Thai government to establish the UCS was the 18 million uninsured people (1). Through the integration of the MWS and VHCS, the UCS eliminated the mistarget and adverse selection issues that these two programs previously faced (1).
Public health service infrastructure has seen large-scale investments from the government in the two decades leading up to UHC.
Since the 1970s, the government of Thailand had invested in local health infrastructure (2). More hospitals were built, and more nurses and doctors were educated; this resulted in the significant improvement of the ratios of population per bed and population per nurse and doctor, as seen in Figure 1 (2). The purpose of this investment was to develop the district health system throughout Thailand; staffing was improved at the district level through the introduction of mandatory rural service for all graduated health professionals, starting with doctors and nurses in 1972 and later covered pharmacists and dentists (2). This investment in local health infrastructure aided in the gradual extension of health coverage in Thailand and set the groundwork for the implementation of UCS by improving physical access to services (2).

Furthermore, to insure proper implementation of Universal Health Care, two rounds of survey (called the Delphi technique), as well as an in-depth interview were conducted among stakeholders before 2001, when UHC was established, for policy formulation. Although the results obtained were limited, it was a good starting point and although the Delphi questionnaire did not provide the expected amount of answers, the in-depth interviews provided more viewpoints from non-health sectors. Five groups were aimed for data collection: the academician, the insurer, the government welfare scheme and policy body, the health care providers and the public at large. While politicians didn’t agree on UHC for the rich, it was concluded that risk protection was a right for all. Also, this research helped establish that a comprehensive package including basic as well as catastrophic illness coverage were necessary. The results of this study were then made available to the Office of Healthcare reform in 2000 and allowed policymakers to establish a policy and finally be used in the political campaign.
Goal of Intervention
The Universal Coverage Scheme is a scheme for all, not just the disadvantaged or the vulnerable. The goal of the Universal Coverage Scheme is “to equally entitle all Thai citizens to quality health care according to their needs, regardless of their socioeconomic status” (2). In order to strengthen the healthcare system, the scheme was intended to shift the focus to primary health care. Primary health care is more cost-effective than outpatient services at hospitals, and lowers the costs of transportation for patients (2).
The UCS has four strategic goals to efficiently provide healthcare for the population. It focuses on curative care, and health promotion and prevention; emphasizes primary health care, and the use of effective and integrated services in a rational manner; promotes proper referral to hospitals; and ensures that the entire population is protected against the catastrophic health expenditures associated with out-of- pocket payments for healthcare services (2).
Description of Intervention
The Universal Coverage Scheme (UCS) aimed to provide equitable entitlement to health care for all Thais (1). Established in 2001 and implemented in 2002, the UCS provided almost-free healthcare coverage for approximately 47 million people (75% of the entire population): the 18 million people that were left previously uninsured and members of the two existing public programs, the MWS and the VHCS. In 2004, UCS beneficiaries were mostly comprised of the poor, with the poorest quintile representing 25% (3). The remaining 25% of the population remained covered under the CSMBS and the SSS (1); 52% of CSMBS beneficiaries and 49% of SSS beneficiaries belonged to the richest quintile (3).
There are three defining features of UCS: a tax-financed scheme with a co-payment of 30 baht ($0.75 USD) per visit or admission; a comprehensive, primary-care focused benefits package; and a fixed annual budget that has a cap on provider payments (1).
The UCS provides a comprehensive benefits package with a focus on primary care, including curative and rehabilitation services, annual check-ups, and health promotion and disease prevention services (1). This includes coverage of inpatient and outpatient services, accident and emergency services, dental care, special investigations, medicines, and medical supplies (1). Clinic-based preventive and health- promoting services were also provided at health centers, thereby filling the gap left by CSMBS and SSS, which did not cover these services (1).
The UCS uses diagnosis-related groups (DRGs), a system that classifies patients based on diagnosis, treatment, and length of hospital stay in order to standardize prospective payment for inpatient services (4). These payments are predetermined, fixed amount, and made to hospitals based on the economic and medical similarity of cases from the previous year (5). Outpatient, disease prevention, and health promotion services covered through the UCS are paid through capitation payments. These are set amounts physicians receive per patient assigned to them, regardless of whether or not the patient seeks care. These capitation payments also serve as deterrents to keep physicians from over-treating patients (4). The UCS requires beneficiaries to receive services from a designated facility. When beneficiaries of the UCS bypass these designated facilities, they must pay 100% of the costs out-of-pocket (OOP) (1). These designated facilities also act as the gatekeeper to refer patients to secondary and tertiary care, thereby preventing utilization of unnecessary specialized health services.
In terms of delivery, the National Health Security Office (NHSO) contracts UCS beneficiaries to providers, such as district hospitals and health centers and pays these providers through contract agreements (6). Providers deliver services to UCS members and submit data back to the NHSO (6). Only 70% of Thailand’s health care facilities are state owned; there are 11,000 publicly-owned clinics and 4,900 privately owned clinics (8). When it comes to hospitals, 75% are run by the Minister of Public Health and the remaining 25% are privately owned (8). As a result, UCS contracts out complex procedures such as heart surgeries or craniotomies to certain private hospitals in urban regions (7). However, many private hospitals are disincentivized from working with UCS due to low reimbursement rates (7). Due to overcrowding and long waiting periods at public facilities, those who can afford private services will choose to access them, thus benefiting the private healthcare industry (8).
Financing
Inadequate funding is the most common obstacle presented as a reason why many countries cannot provide universal health coverage to its citizens. Nevertheless, Thailand, a middle-income country, has established UCS, without the wealth of a high-income country. Initial strides to establish universal healthcare coverage in the country was made in 2001 through the 30 Baht health scheme program, whereby no patient was required to pay more than 30 baht per visit (9). However, this program was abolished in 2006 for political motivations, then reimplemented in 2012 with exceptions that include emergency, prevention, promotion, visits without prescriptions and visits to health centers below the community level (10).
Thailand’s total health expenditure is 3.7% of its GDP, for an annual budget of 153,152 million baht (4,646 million USD) (11). Completely funded by general taxes, 40.2% of the annual budget funds the UCS and the remaining 59.8% funds the SSS and CSMBS (10). Through this funding, UCS provides coverage for 73.71% of Thailand’s population (11).
The national health expenditure is split between government, including UCS, and private health expenditure. While private health expenditure comprised the majority of the nation’s health expenditure in 1994, by 2013 the ratio of government to private expenditure was 77% to 23% (11). From 2005 to 2010, UCS’s budget continued to increase from 5.41% to 6.94% of total Thai governmental budget (11). This budget included all health expenditures and the salaries of governmental health staff (11).
Metrics of Evaluation
Four metrics of evaluation were chosen to evaluate the UCS. The first metric was patient utility of the UCS, and reasons for not utilizing. The inpatient and outpatient utilization rates indicate the number of beneficiaries accessing the services available to them. Understanding the reasons that beneficiaries do not utilize these services may provide insight to the weaknesses of the UCS and identify areas for improvement.
The second metric was the rate of catastrophic health expenditure. This is defined as the out-of-pocket spending for healthcare exceeding a certain proportion of a household’s income (15). Evaluating the UCS through rate of catastrophic health expenditure incurred by its beneficiaries enables the measurement of the incidence of financial hardship caused by health payments. It also offers insight into the disparities in accessing healthcare that still exist after implementation of the UCS.
Health status indicators such as life expectancy, vaccine coverage, and infant mortality rate were used as the third metric of evaluation. These indicators provide a more detailed assessment of the health status of the population, and can also be used to evaluate the overall health performance of the country.
The distribution of healthcare professionals was the fourth metric of evaluation. The distribution affects a healthcare system’s ability to deliver essential health services to all beneficiaries in different regions. This metric not only demonstrates a healthcare system’s capability of providing coverage, but showcases the disparity that exists between regions as well.
The final metric used to evaluate the UCS was the quality of care provided by the scheme. In order to do so, patient satisfaction was used as an indicator of quality of care to measure how successful the UCS was in providing care. It provides the patient’s perspective of their experience with the system, and can provide guidance for necessary improvements to the healthcare system.
Impact
Healthcare service utilization
Overall, there has been an increase in both inpatient and outpatient healthcare service utilization across the country from 2003- 2015 (2). However, when surveyed by the International Health Policy Program and National Statistical Office, reasons for unmet needs were those disproportionately affecting the rural poor, such as too far to travel and service not covered by benefit package (2,15).
Figure E: (15)
Figure 12: (15)
Rate of catastrophic health expenditure
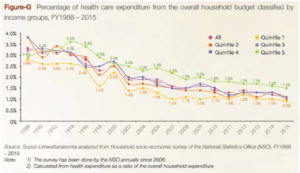
As seen in figure G, the percentage of household budget spent on healthcare has dramatically decreased for all quintiles from 1988-2015 (15). Indeed, according to data from The World Bank, the number of households pushed below the poverty line due to out-of-pocket healthcare expenditures dramatically decreased from 183,000 in 1996 to 83,000 in 2010 (16). However, this impact was disproportionately distributed between urban and rural regions. Figure 15 shows a map of Thailand and the rate of catastrophic health expenditure per 100 households in 1996, prior to USC implementation, 2002, at the beginning of UCS implementation and in 2008, 7 years after the implementation of UCS (2). From this map, we see that the catastrophic health expenditure has decreased in almost all provinces. However, the province of Surin, a vastly rural poor area, shows an increase in household health impoverishment.
Figure G: (15)
Figure 15: (2)
Health indicators
Thailand’s life expectancy has increased steadily since the implementation of the UCS: from 70.8 years in 2001, one year prior to implementation, it has risen to 75.3 years in 2016 (17). According to the Primary Health Care Performance Initiative (PHCPI), Thailand had the highest DTP3 coverage of all low- and middle-income countries (LMICs) in 2017, with 99% of one- year-olds receiving three doses of the combined diphtheria, tetanus toxoid, and pertussis vaccine (18).
In addition, the infant mortality rate in Thailand has been on the decline (19), most likely due to the synergistic effects of the UCS and development. However, the rural-urban mortality rate ratio has increased from 1.3 in 1964 to 1.8 in 2005 (20). This increase indicates that the infant mortality rate has fallen much slower in rural regions compared to urban regions.
Figure 3: (14)
Distribution of healthcare professionals
In 2009, more rural residents were covered under UCS than urban residents (21). However, when the distribution of healthcare professionals is observed, there is an obvious skew of more healthcare professionals in urban areas; only 18% of doctors served in rural areas in 2017 (22). This staggering difference between the rural and urban distribution can be attributed to the brain-drain of healthcare professionals both from rural to urban areas, and from public to private hospitals due to higher quality of life and pay respectively.
Figure 5: (22)
Quality of Care
Rates of satisfaction amongst UCS beneficiaries has been steadily increasing since 2002, reaching 90% in 2015 (Figure 52-(15)). According to a 2012 study from KhonKaen University in Thailand, the sense of wellbeing amongst villagers in the rural Northern Region increased significantly after the implementation of UCS, further contributing to the overall sense of security (23). Despite these positive results, around 30% of card holding villagers never utilized UCS services, and 20% of card- using villagers reported dissatisfaction; these percentages are significantly higher than the overall country averages (23). In addition, the number of complaints concerning quality of care for lack of service, inconvenience, being charged and substandard care remained relatively constant from 2011-2015 (Figure 51-(15)). These are all factors that disproportionately affect the rural poor, once again confirming the lack of improvement in quality of care in rural areas.
Figure 7: (2)
Figure 52: (15)
Figure 51: (15)
Why It Worked and Why It Did Not
Why it worked
The first reason for the success of the UCS in Thailand was the strong leadership behind its implementation. The Thai Rak Thai party used the promise of a universal healthcare scheme in their 2001 electoral campaign and continued to push for its implementation during their mandate (24). Hence, there was strong advocacy and political effort to adopt a universal health system coverage. There was also continuity, as the subsequent leaders of Thailand worked to keep the momentum going (24).
Secondly, the implementation of UCS was a result of Thailand’s ongoing effort to strengthen its health system—notably through investment in rural medical facility infrastructures (25). Therefore, not only did UCS increase access to healthcare services, it provided patients with an increased quality of care as a result of this investment (25). Finally, a tax-financed scheme ensured the percentage of country’s GDP spent on healthcare would not increase (26). In other words, the Thai government was able to extend healthcare coverage to more citizens without a significant increase on its current spending on healthcare.
All in all, the reason of success of Thailand’s UCS can be best described by a quote of Prateep Tanakijjaroen, Acting Secretary-General of the NHSO: “Finally, the participation of every stakeholder is still the most important mechanism moving the universal health coverage scheme towards its ultimate goal. With strength and cooperation we can we can all have a brighter, happier future” (15).
Challenges still faced
With strong evidence of an overall improvement of health conditions in Thailand, the UCS has been rightfully praised. However, the program is still facing challenges, notably in sustainability and equity. The fact that Thailand had not increased overall spending on healthcare after implementation of UCS has been cited as a reason for the success of the program, but this also calls into question its financial sustainability (11). Indeed, clinicians expressed concerns regarding the inadequately small allocated budget of $31.63 per registered person per year in inpatient care (26). Moreover, the overall reallocation of resources, based on population density, that came with the implementation of UCS was originally intended to reduce rural- urban inequities; instead, this led to financial troubles for more than 30% of UCS hospitals, small rural community hospitals in the north and northeast being overly affected by this issue (26). This new allocation of resources led to small rural villages having insufficient budgets due to small population size, which further deepened urban/rural inequities (26).
Overall, Thailand’s Universal Coverage Scheme did manage to attain its goals with the help of strong political and population support, however there is a need of a stronger financing scheme as well as focus on rural inequities to ensure the long-term success of the project (26).
Future Implications
The UCS was well-received by the people of Thailand, as seen by its high satisfaction rates. However, for it to be sustainable, UCS must establish and adhere to strict financial targets. Currently, the funding of UCS is renegotiated with the Ministry of Health every year (6). This jeopardizes the sustainability and improvement of the system.
Related to the lack of consistent funding, the adequacy of the funding is also an issue. Currently, the Thailand government does not spend the 5% of their GDP recommended by the World Health Organization (WHO) that is necessary to sustain a universal healthcare plan (27). This could potentially be one the biggest reasons for inequality between rural and urban regions. Additional funding is also necessary to support policy research into understanding the changing needs of the population. There are worries that the current funding will not be able to sustain the aging population and rising expectation of UCS beneficiaries (15). Indeed, Thailand is projected to enter a health crisis in 2025 unless significant changes are made and funding is increased (2,28). A possible solution to this could be to implement increased taxes on tobacco and alcohol, which could lead to healthier practices while also providing the government with a constant source of revenue. Such a strategy would increase UCS’s funding by 0.64% of the GDP, allowing Thailand to continue towards the 5% minimum (4).
Figure 10: (15)
Finally, as discussed in this study, distribution of healthcare resources between rural and urban regions needs to be improved, particularly with regards to healthcare professionals. The fact that only 18% of doctors work in rural areas is an obvious sign of need for improvement (22). Policies can be implemented to incentivize healthcare professionals to work in rural regions such as recruiting students from rural areas, higher pay, or subsidizing student loans.
Conclusions
The achievements and handicaps of Thailand’s universal coverage scheme serve as an example for other countries in the global health community that wish to achieve universal health
coverage. With the successful implementation of UCS, Thailand has proved that universal health coverage is possible in an LMIC setting, which has the potential to provide guidance for other countries with similar economic statuses.
An important lesson learned from Thailand’s success is that universal health coverage cannot be achieved without the cooperation of multiple agencies; this includes strong political commitments, reliable policy research and public interest. Without the Thai Rak Thai party’s advocacy for universal healthcare coverage throughout their electoral campaign and mandate, the UCS likely would not have been implemented as early as 2001.
The establishment of healthcare infrastructure at the rural level is essential to the successful implementation of a scheme like UCS. Through years of investment in building district hospitals and centers and implementing a policy of mandatory rural service for health professional graduates prior to the establishment of UCS, the scheme was able to be implemented at the rural level (2). Despite these efforts, this case study has shown that disparities between the urban and rural populations continue to exist within UCS. Indeed, there needs to be work done to close these gaps and create an equitably- distributed healthcare coverage scheme.
Acknowledgements
We would like to extend our sincerest thanks to Dr. Seung Chun Paek, Assistant Dean for Research and International Relations at Mahidol University, Thailand for providing his expertise and guidance while preparing this case study. We would also like to thank Dr. Madhukar Pai for his inspiration and leadership throughout the semester, as well as Hannah Alsdurf for her advice in refining our final case study.
References
- Meemon N, and Paek SC. Health- Seeking Behaviour of the Uninsured Before and After the Universal Coverage Scheme in Thailand. APSSR [Internet]. 2018 [October 15 2015]; 18(1): 1-14. Available from: http:// apssr.com/wp-content/uploads/2018/06/ RA-1-revised.pdf
- Evans TG, Chowdhury A, Evans D, Fidler A, Lindelow M, Mills A, & Scheil- Adlung X. Thailand’s Universal Coverage Scheme: Achievements and Challenges [October 20 2018]. 2012 May [ACCESS DATE];1-120. Available from: http://www. jointlearningnetwork.org/uploads/files/ resources/book018.pdf
- Tangcharoensathien V, Prakongsai P, Limwattananon S, Patcharanarumol W, & Jongudomsuk P. (2007). Achieving universal coverage in Thailand: What Lessons Do We Learn?. Health Systems Knowledge Network [Internet]. 2007 March [October 27 2018]; 1-25. Available from: http://www. who.int/social_determinants/resources/ csdh_media/universal_coverage_thailand_2007_en.pdf
- Antos JR. Health Care Financing in Thailand: Modeling & Sustainability. Mission Report to the World Bank [Internet]. 2007 August [October 15 2018]; 1-22 .Available from: http://siteresources.worldbank. org/INTTHAILAND/Resources/333200- 1182421904101/2007aug-health-financing- modeling.pdf
- Mathauer I & Wittenbecher F. Hospital Payment Systems Based on Diagnosis- Related Groups: Experiences in Low-and Middle-Income Countries. Bull World Health Orga [Internet] 2013 August [November 20 2018]; 91:746-756A . Available from: http://www.who.int/ bulletin/volumes/91/10/12-115931/en/
- Patcharanarumol W, Panichkriangkrai W, Sommanuttaweechai A, Hanson K, Wanwong Y, Tangcharoensathien V. Strategic Purchasing and Health System Efficacy: A Comparison of Two Financing Schemes in Thailand. PLoS One [Internet] 2018 April [November 29 2018]; 13(4):1-13 Available from: https://journals.plos.org/ plosone/article/file?id=10.1371/journal. pone.0195179&type=printable
- Srithamrongsawat S. Private hospitals under health insurance schemes in Thailand. [Internet] 2014 November. COOPAMI [November 30 2018]; Available from: http:// http://www.coopami.org/en/countries/countries/ thailand/projects/2014/pdf/2014110307. pdf
- Sathapongoakdee P. Thailand Industry Outlook 2016-18: Private Hospital Industry. Krungsri Research [Internet] 2016 June [November 30 2018]; Available from: https://www.krungsri.com/bank/ getmedia/9edb9946-cb72-4e47-bed8- 91d9b38a0a78/IO_Hospital_2016_ EN.aspx
- Damrongplasit K, & Melnick GA. Early Results from Thailand’s 30 Baht Health Reform: Something to Smile About. Health Affairs [November 4 2018] 2009 [ACCESS DATE]: 28(3): Available from: https:// http://www.healthaffairs.org/doi/pdf/10.1377/ hlthaff.28.3.w457
- Damrongplasit K. & Melnick G. Funding, Coverage, and Access Under Thailand’s Universal Health Insurance Program: An Update After Ten Years. Applied Health Economics and Health Policy [Internet] 2015 [October 15 2018] 13(2), 157-166. DOI 10.1007/s40258-014- 0148-z
- Global Health Expenditure Database. WHO [Internet] [November 30 2018] Available from: http://apps.who.int/nha/ database/ViewData/Indicators/en
- SomkotraT&LagradaLP.Paymentsfor Health Care and Its Effect on Catastrophe and Impoverishment: Experience from the Transition to Universal Coverage in Thailand. Social Science & Medicine [Internet] 2006 [November 23 2018]; 67(12): 2027-2035 Available from: https:// http://www.ncbi.nlm.nih.gov/pubmed/18952336
- Li C, Yu X, Butler JRG, Yiengprugsawan V, Yu M. Moving Towards Universal Health Insurance in China: Performance, Issues and Lessons from Thailand. Social Sci Med [Internet] 2011 June [November 18 2018];73(3): 359-366 Available from: https:// http://www.ncbi.nlm.nih.gov/pubmed/21733610
- Jongudomsuk P et al. The Kingdom of Thailand Health System Review. Asia Pacific Observatory on Health Systems and Policies [Internet] 2015 [December 3 2018]; 5(5) Available from: http://iris.wpro.who.int/ bitstream/handle/10665.1/11359/9789290617136_e
- NHSO Annual Report Fiscal Year 2015.NHSO [Internet][November 29 2018];1-104 Available from: https:// http://www.nhso.go.th/eng/files/userfiles/ file/2018/001/Annual%20report%20 2015.pdf?fbclid=IwAR1krM- PgNUQwH0JA7f7bkRFQs1R- U5DEbzolFcuGxp6eqa04B24qkvo4Kw
- Wagstaff A, Flores G, Smitz MF, Hsu J, Chepynoga K, Eozenou P. Progress on Impoverishing Health Spending: Results for 122 Countries. Lancet Global Health [Internet] 2017 December [November 30 2018];6(2): 180-192 Available from: https:// data.worldbank.org/indicator/SH.UHC. NOP1.
- Life Expectancy at Birth, Total (Years). The World Bank [Internet] 2017 [November 29 2018] Available from: https://data. worldbank.org/indicator/SP.DYN.LE00. IN?locations=TH&start=2001
- Thailand PHCPI. [Internet][Publisher Unknown]:[date unknown][November 29 2018] Available from: https://improvingphc. org/east-asia-pacific/thailand
- Mortality rate, infant (per 1,000 live births) [Internet][The World Bank]: https://data.worldbank.org/indicator/ SP.DYN.IMRT.IN?view=chart
- Yiengprugsawan V, Carmichael GA, Lim LLY, Seubsman S, Sleigh AC. Has Universal Health Insurance Reduced Socioeconomic Inequalities in Urban and Rural Health Service Use in Thailand?. Health Place [Internet] 2010 September [November 24 2018]; 16(5):1030-1037 Available from: https://www.ncbi.nlm.nih. gov/pmc/articles/PMC3031979/
- Thailand Health Profile. MoPH[Internet] 2008 [November 22 2018] 302-309 Available from: http://wops.moph. go.th/ops/thp/images/stories/Report_pics/ CD_ROM53/Eng/Chapter6.5.pdf
- Woratanarat T, Woratanarat P, Lekthip C. Primary health care systems (PRIMASYS): Case Study from Thailand, Abridged Version. WHO [Internet] 2017 [November 25 2018] Licence: CC BY- NC-SA 3.0 IGO. Available from: http:// http://www.who.int/alliance-hpsr/projects/ alliancehpsr_thailandabridgedprimasys. pdf
- Mee-Udon F.Universal Health Coverage Scheme Impact on Well-Being in Rural Thailand. International Journal of Health Care Quality Assurance [Internet] 2014 [November 21 2018]; 27(6): 456-467 Available from: https:// doi.org/10.1108/ IJHCQA-11-2012-0111
- Tangcharoensathien V, Pitayarangsarit S, Patcharanarumol W, Prakongsai P, Sumalee H, Tosanguan J, Mills A. Promoting Universal Financial Protection: How the Thai Universal Coverage Scheme was Designed to Ensure Equity. Health Research Policy and Systems. [Internet] 2013 August [November 22 2018];11(25): Available from: https:// health-policy-systems.biomedcentral.com/ articles/10.1186/1478-4505-11-25
- Wibulpolprasert S.Thailand’s Health Ambitions Pay Off. Bull World Health Organ [Internet] 2014 July [November 14 2018]; 92(7): 472-473 Available from: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4121874/
- Thaiprayoon S, & Wibulpolprasert S. Political and Policy Lessons from Thailand’s UHC Experience. Observer Research Foundation. [Internet] 2017 April [November 29 2018];174:Available from. (https://www.orfonline.org/wp-content/ uploads/2017/04/ORF_IssueBrief_174_ ThailandUHC.pdf
- Arguing for Universal Health Coverage. World Health Organization [Internet] 2013 [November 30 2018] Available from: https://www.who.int/health_financing/ UHC_ENvs_BD.PDF
- Nishiura H, Barua S, Lawpoolsri S, Kittitrakul C, Leman MM, Maha M, Muangnoicharoen S. Health inequalities in Thailand: Geographic Distribution of Medical Supplies in the Provinces. The Southeast Asian Journal of Tropical Medicine and Public Health [Internet] 2004 [22 November 2018]: 35: 735-40 Available from: https://www.researchgate.net/ publication/8043644_Health_inequalities_ in_Thailand_Geographic_distribution_of_ medical_supplies_in_the_Provinces